Free Premium NAPLEX® Practice Questions
Practice with questions written by pharmacists to reflect the NAPLEX in both format and difficulty, because if practice feels like the exam, the real thing will feel like practice.
NAPLEX Sample Practice Questions
MK is a 69-year-old male visiting his primary care provider for a routine follow-up. He reports chronic pain in his right knee that has become worse in the last few months and is limiting his physical activity. The patient alternates taking Advil and Tylenol around the clock to make the pain tolerable.
Past Medical History: osteoarthritis, hypertension, dyslipidemia
Allergies: NKDA
Medications:
Advil 400 mg every 6 hours as needed for pain
Benicar HCT 40
mg/25 mg
once daily
Lipitor 20 mg once daily
Tylenol 650 mg every 6 hours as needed for pain
Vital Signs: BP 139/84 mmHg, HR 75 bpm, RR 15 bpm, Ht 5′ 11″, Wt 85 kg
Laboratory Tests:
Sodium 135 mEq/L
Potassium 4.2 mEq/L
Chloride 98
mEq/L
Bicarbonate 19 mEq/L
Blood urea nitrogen 35 mg/dL
Serum creatinine 1.1 mg/dL
Assessment and Plan:
1. Osteoarthritis: pain limiting activity; refer to
orthopedic
surgeon for evaluation with goal to decrease NSAID use.
2. Hypertension: BP above goal; titrate
therapy
to optimize current BP while decreasing NSAID use.
3. Follow-up in 1 month for BP assessment.
The addition of which antihypertensive medication is most appropriate for this patient?
| A. | Chlorthalidone | ||
| B. | Hydralazine | ||
| C. | Lopressor | ||
| D. | Lotensin | ||
| E. | Procardia XL |
Explanation:
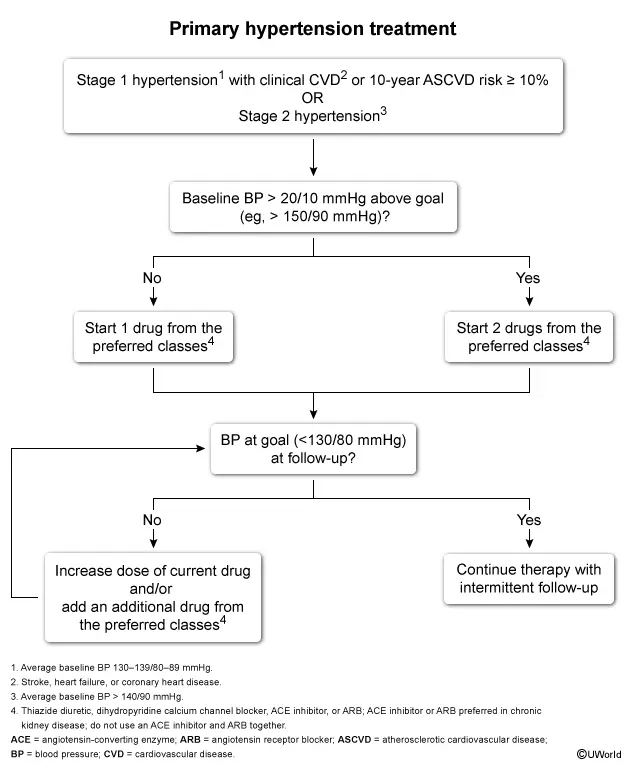
This patient’s BP is above goal (eg, ≥ 130/80 mmHg) despite his current treatment with a combined thiazide diuretic and angiotensin receptor blocker (ARB) [eg, Benicar HCT (olmesartan/hydrochlorothiazide)]. This is likely related to multiple modifiable risk factors (eg, NSAID use, limited physical activity) but warrants medication titration (eg, adding a drug from a different preferred drug class, increasing the dose of the current drug).
Preferred antihypertensive drug classes include thiazide diuretics, dihydropyridine calcium channel blockers (DHP CCBs), angiotensin-converting enzyme (ACE) inhibitors, and ARBs. Because this patient is already taking an ARB and a thiazide diuretic, adding a DHP CCB [eg, Procardia XL (nifedipine extended-release)] is recommended. Follow-up and medication adjustment should continue monthly until goal BP is achieved.
(Choice A) The addition of a thiazide diuretic (eg, chlorthalidone) is not appropriate because it is a duplication of the current hydrochlorothiazide therapy.
(Choice B) Direct vasodilators (eg, hydralazine) are not a preferred antihypertensive drug class due to adverse effects (eg, reflex tachycardia, peripheral edema); they are generally reserved for resistant hypertension and hypertensive crises.
(Choice C) Because beta-blockers [eg, Lopressor (metoprolol tartrate)] are less effective at lowering BP, their use should be limited to patients with specific comorbidities (eg, heart failure, coronary artery disease).
(Choice D) ACE inhibitors [eg, Lotensin (benazepril)] should not be used in combination with ARBs due to their overlapping mechanism of action (eg, renin-angiotensin-aldosterone system inhibition) and increased risk of hyperkalemia and renal impairment.
Things to remember:
Antihypertensive therapy should be titrated (eg,
adding a drug from a different preferred drug class, increasing the dose of the current
drug) to achieve a BP goal < 130/80 mmHg.
- Refer to the latest version of the RxPrep Course Book – Hypertension chapter, “Treatment Principles (ACC/AHA)”, beginning on page 409.
- Treatment Principles (ACC/AHA)
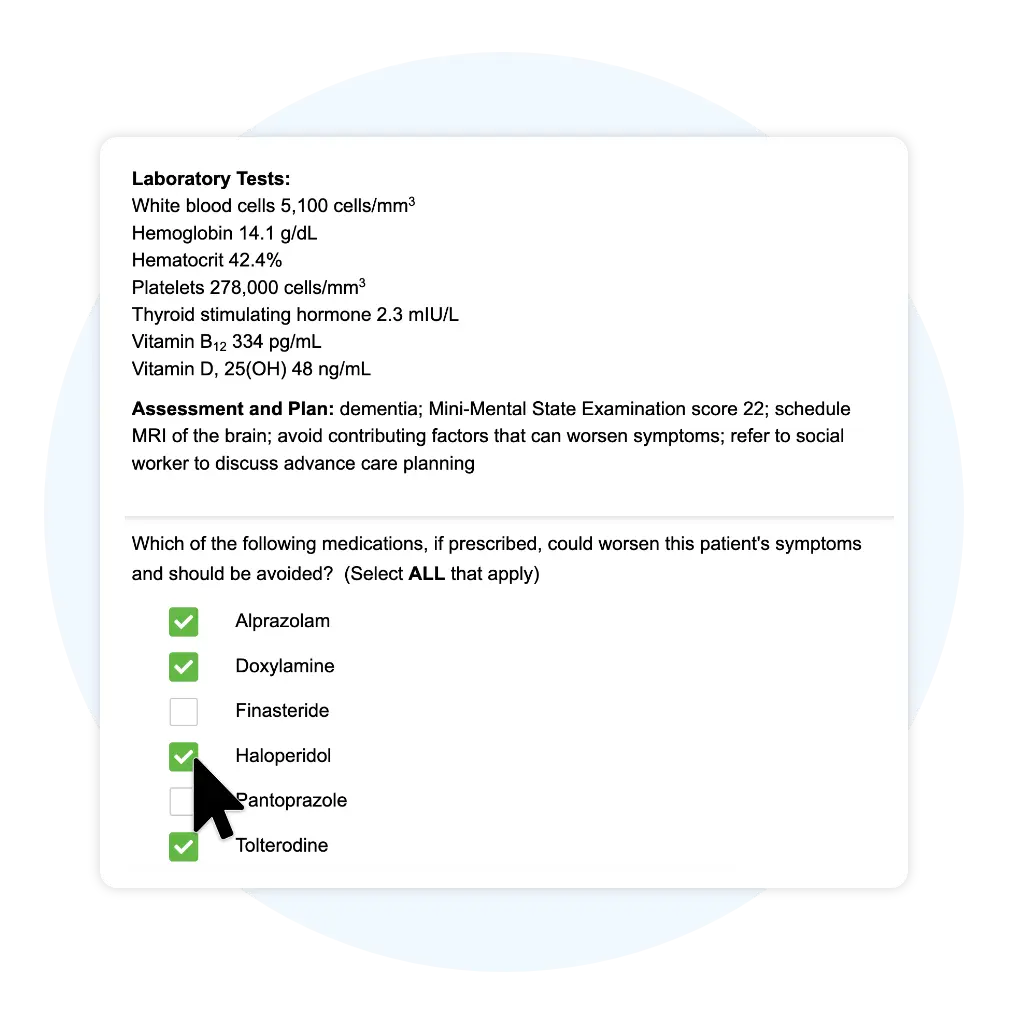
JC is a 74-year-old male who is brought to the office by his son due to increasing forgetfulness. The son reports that his father asks the same question multiple times and that he recently got lost while driving to the grocery store.
Past Medical History:
Dyslipidemia
Heart failure (ejection fraction
35%)
Hypertension
Myocardial infarction (4 years ago)
Type 2 diabetes mellitus
Medications:
Aspirin 81 mg PO daily
Atorvastatin 40 mg PO
daily
Carvedilol 25 mg PO BID
Empagliflozin 10 mg PO daily
Furosemide 20 mg PO
daily
Nitroglycerin 0.4 mg sublingual as directed
Sacubitril 49 mg/valsartan 51 mg PO
BID
Spironolactone 25 mg PO daily
Vital Signs: BP 112/64 mmHg, HR 55 bpm, RR 17 bpm, T 97.4°F (36.3°C), Ht 5′ 10″, Wt 183 lbs
Laboratory Tests:
White blood cells 5,100 cells/mm3
Hemoglobin
14.1 g/dL
Hematocrit 42.4%
Platelets 278,000 cells/mm3
Thyroid stimulating
hormone 2.3 mIU/L
Vitamin B12 334 pg/mL
Vitamin D, 25(OH) 48 ng/mL
Assessment and Plan: dementia; Mini-Mental State Examination score 22; schedule MRI of the brain; avoid contributing factors that can worsen symptoms; refer to social worker to discuss advance care planning
Which of the following medications, if prescribed, could worsen this patient’s symptoms and should be avoided? (Select ALL that apply)
| A. | Alprazolam | ||
| B. | Doxylamine | ||
| C. | Finasteride | ||
| D. | Haloperidol | ||
| E. | Pantoprazole | ||
| F. | Tolterodine |
Explanation:
| Medications that worsen dementia | |
|
Antipsychotics
|
|
|
Central nervous system depressants
|
|
|
Drugs with anticholinergic properties
|
|
This patient has new signs of dementia, including forgetfulness and getting lost in a familiar place. Select drugs can worsen dementia symptoms or cause reversible confusion and are included on the Beers Criteria list of potentially inappropriate medications that should be avoided in most older adults.
Drugs that should be avoided in patients with dementia include:
-
Central nervous system (CNS) depressants, which can cause sedation and confusion with short- and long-term use. This includes opioids (eg, morphine) and benzodiazepines (eg, alprazolam) (Choice A).
-
Anticholinergics, such as antihistamines (eg, doxylamine) and antimuscarinic agents used for urinary incontinence (eg, tolterodine). These drugs antagonize acetylcholine, a neurotransmitter involved with memory, attention, and learning (Choices B and F).
-
Antipsychotics (eg, haloperidol), which increase the rate of cognitive decline due to mechanisms that are not well defined. Antipsychotics may be used in select patients with dementia-related psychosis, but because of a boxed warning for increased mortality, they are reserved for use when nonpharmacologic strategies fail (Choice D).
(Choice C) Finasteride (a 5-alpha reductase inhibitor) is a treatment for benign prostatic hyperplasia. Its most common adverse effect is sexual dysfunction (eg, impotence, decreased libido); it does not cause CNS adverse effects.
(Choice E) Proton pump inhibitors (eg, pantoprazole) are not known to cause delirium or altered mental status, unlike histamine-2 receptor antagonists (eg, famotidine), which can impair cognition in elderly patients or patients with renal dysfunction.
Things to remember:
Antipsychotics, central nervous system depressants,
and drugs with anticholinergic effects can impair cognition and should be avoided in
patients with dementia.
- Refer to the latest version of the RxPrep Course Book – Alzheimer’s Disease chapter, “Key Drugs that Can Worsen Dementia”, beginning on page 840.
- Key Drugs that Can Worsen Dementia
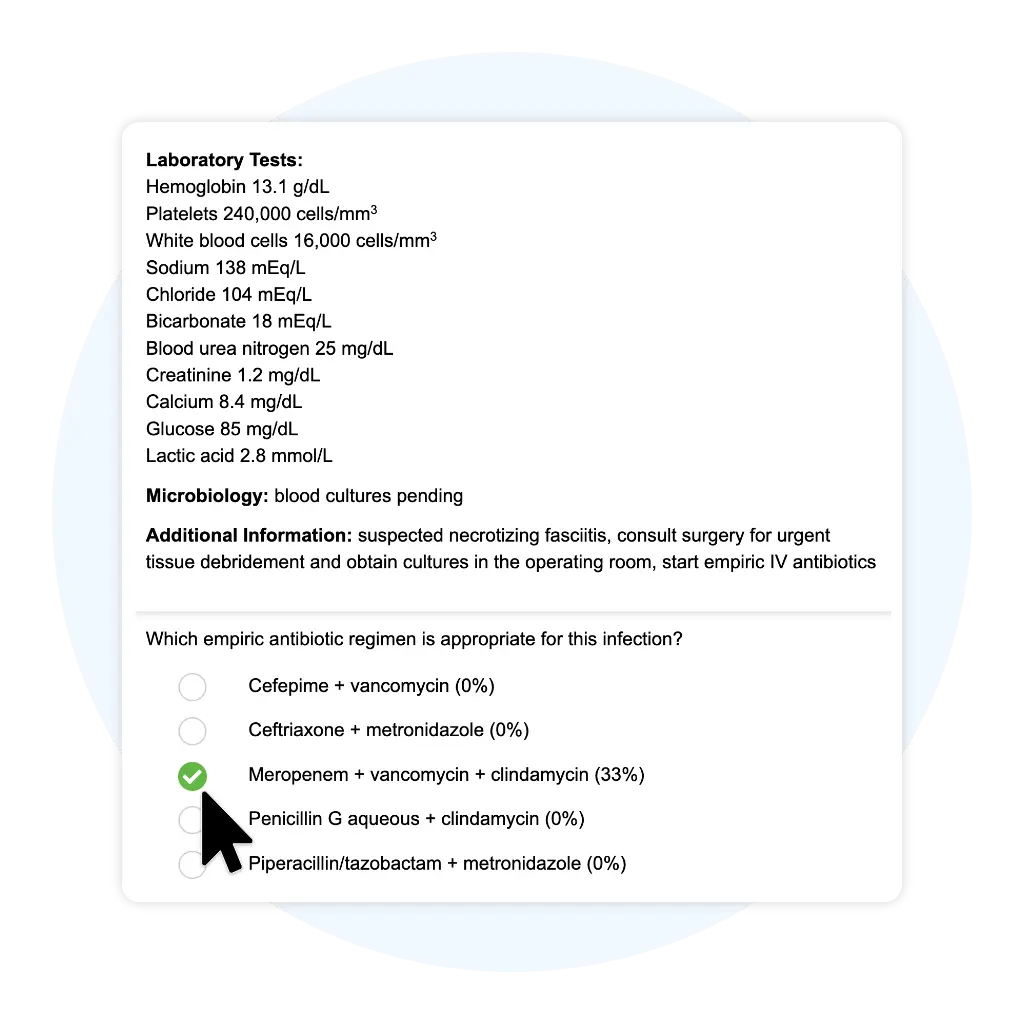
PT is a previously healthy 32-year-old female who comes to the emergency department with severe pain in her right lower leg. She reports getting an infection from a cut that occurred while hiking in the woods two days ago. The infection has spread quickly and become extremely painful in the last 24 hours.
Allergies: NKDA
Home Medications: none
Vital Signs: BP 95/60 mmHg, HR 110 bpm, RR 18 bpm, O2 sat 96% (room air), T 102.4°F (39.1°C), Ht 5′ 4″, Wt 58 kg, pain 10/10 (right lower leg)
Physical Exam: right lower extremity with significant erythema without sharp margins, edema extending beyond the border of erythema, and some areas with a purple discoloration of the skin; the area is hardened with pain disproportionate to its appearance
Laboratory Tests:
Hemoglobin 13.1 g/dL
Platelets 240,000
cells/mm3
White blood cells 16,000 cells/mm3
Sodium 138
mEq/L
Chloride 104 mEq/L
Bicarbonate 18 mEq/L
Blood urea nitrogen 25
mg/dL
Creatinine 1.2 mg/dL
Calcium 8.4 mg/dL
Glucose 85 mg/dL
Lactic acid 2.8
mmol/L
Microbiology: blood cultures pending
Additional Information: suspected necrotizing fasciitis, consult surgery for urgent tissue debridement and obtain cultures in the operating room, start empiric IV antibiotics
Which empiric antibiotic regimen is appropriate for this infection?
| A. | Cefepime + vancomycin | ||
| B. | Ceftriaxone + metronidazole | ||
| C. | Meropenem + vancomycin + clindamycin | ||
| D. | Penicillin G aqueous + clindamycin | ||
| E. | Piperacillin/tazobactam + metronidazole |
Explanation:
| Necrotizing fasciitis | |
|
Microbiology
|
|
|
Pathogenesis
|
|
|
Clinical manifestations
|
|
|
Treatment
|
|
| MRSA = methicillin-resistant Staphylococcus aureus. | |
Necrotizing fasciitis (NF) is a life-threatening skin and soft tissue infection that leads to the destruction of muscle fascia and overlying subcutaneous fat. The initial presentation is similar to cellulitis (eg, erythema, edema), but rapidly progresses to red-purple skin discoloration and necrosis. Other distinguishing characteristics include wooden-hard induration, pain that is more severe than expected based on the appearance, and systemic toxicity (eg, fever, hypotension).
NF requires urgent surgical debridement and broad-spectrum antibiotics. The infection can be monomicrobial or polymicrobial; possible pathogens include group A Streptococcus, Staphylococcus aureus [including methicillin-resistant S. aureus (MRSA)], Enterobacteriaceae, and anaerobes (gram-positive and gram-negative). Appropriate empiric treatment regimens to target these organisms include meropenem or piperacillin/tazobactam in combination with vancomycin or daptomycin. Clindamycin is often added empirically to inhibit streptococcal toxin production.
(Choice A) Cefepime (a fourth-generation cephalosporin) and vancomycin both lack the necessary activity against anaerobic organisms.
(Choices B and E) Piperacillin/tazobactam or ceftriaxone combined with metronidazole do not provide the needed activity against MRSA. Ceftriaxone (a third-generation cephalosporin) is also not a preferred beta-lactam for empiric NF treatment because its activity is too narrow. In addition, because piperacillin/tazobactam has intrinsic activity against anaerobes, there is no benefit to adding metronidazole.
(Choice D) Penicillin G aqueous is too narrow for initial empiric therapy but may be warranted for definitive therapy, with clindamycin, if cultures identify a monomicrobial infection with Streptococcus pyogenes or Clostridium spp.
Things to remember:
Necrotizing fasciitis is a rapidly progressing and
life-threatening skin and soft tissue infection. Treatment requires urgent surgical
debridement and broad-spectrum antibiotics (meropenem or piperacillin/tazobactam in
combination with vancomycin or daptomycin). Clindamycin can be added empirically to suppress
streptococcal toxin production.
- Refer to the latest version of the RxPrep Course Book – Infectious Diseases II: Bacterial Infections chapter, “Severe Skin and Soft Tissue Infections”, beginning on page 354.
- Severe Skin and Soft Tissue Infections
MH is a 63-year-old female with hypertension, chronic kidney disease, and degenerative joint disease. She is 5’3”, weighs 135 lbs, and has a serum creatinine of 2.5 mg/dL at the time of admission for hip replacement surgery. The provider orders enoxaparin 30 mg SC every 12 hours for deep vein thrombosis prophylaxis to start post-operatively. Which of the following actions is most appropriate for the pharmacist to take?
| A. | Dispense the enoxaparin order as written. | ||
| B. | Contact the provider and recommend enoxaparin 30 mg SC every 24 hours. | ||
| C. | Contact the provider and recommend enoxaparin 30 mg IV every 12 hours. | ||
| D. | Contact the provider and recommend enoxaparin 40 mg SC every 12 hours. | ||
| E. | Contact the provider and recommend enoxaparin 60 mg SC every 24 hours. |
Explanation:
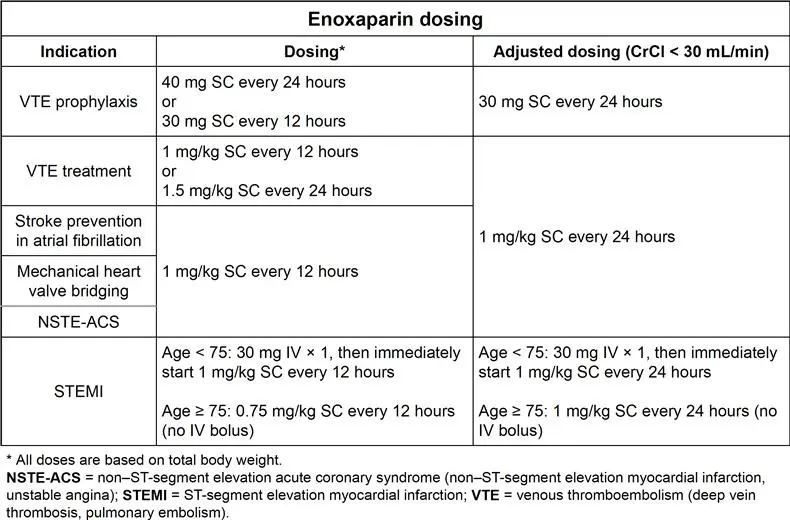
Anticoagulants are used to prevent venous thromboembolism (VTE) in high-risk patients. Enoxaparin, a low molecular weight heparin (LMWH), is the preferred medication for VTE prophylaxis in most patients based on its efficacy, frequency of administration, and partial reversibility with protamine.
The enoxaparin dose used for VTE prophylaxis is lower than the dose used to achieve therapeutic anticoagulation. The regimen is modified in patients with severely decreased kidney function to prevent accumulation and possible bleeding. To identify the most appropriate dosing regimen for a patient:
1. Calculate the patient’s creatinine clearance (CrCl) using ideal body weight (IBW)
2. Determine the best dosing regimen based on the patient’s CrCl
- CrCl ≥ 30 mL/min: 40 mg subcutaneously (SC) every 24 hours or 30 mg SC every 12 hours
- CrCl < 30 mL/min: 30 mg SC every 24 hours
(Choice A) Enoxaparin 30 mg SC every 12 hours would be correct if the patient’s CrCl was 30 mL/min or greater. The administration frequency should be every 24 hours based on this patient’s creatinine clearance (CrCl 19 mL/min).
(Choice C) Enoxaparin is administered subcutaneously, not intravenously, for VTE prophylaxis. In addition, it should be administered every 24 hours for a CrCl less than 30 mL/min.
(Choice E) This dose and frequency (1 mg/kg SC every 24 hours) would be correct for the treatment of a VTE in a patient with a CrCl < 30 mL/min, not for VTE prophylaxis.
Things to remember:
Enoxaparin is a renally eliminated medication that
is preferred for VTE prophylaxis in most patients. The standard doses are 40 mg SC every 24
hours or 30 mg SC every 12 hours; the dose is 30 mg every 24 hours when the CrCl is less
than 30 mL/min.
- Refer to the latest version of the RxPrep Course Book – Anticoagulation chapter, “Low Molecular Weight Heparins”, beginning on page 475.
- Low Molecular Weight Heparins
A pharmacist is approached by a prescriber for help writing a parenteral nutrition order. The patient is currently receiving a 2-in-1 formula consisting of 425 grams of dextrose and 110 grams of protein.
“Patient needs 2,400 calories per day. Recommend 10% Intralipid infusion to provide the remaining calories”.
Explanation:
Correct Answer : 39
The current PN provides 1885 kcals, so 515 kcals must be provided by the 10% Intralipid. 515 kcals x 1 mL/1.1 kcals = 468.1818 mL of 10% Intralipid. Be sure to divide the volume of 10% Intralipid by 12 to get the 12-hr infusion rate. In many hospitals, lipids are infused over 8 or 12 hours.
- Refer to the latest version of the RxPrep Course Book – Calculations III: Parenteral & Enteral Nutrition chapter, “Fat”, beginning on page 146.
- Fat
Want to keep practicing?
Explore NAPLEX Question Format
Why More Students Choose UWorld RxPrep
Exam-Like Practice
Exam-Like
Practice
Detailed Reporting
Customizable Practice Tests
Join the Thousands Who Will Pass with UWorld RxPrep
Learn More about the NAPLEX

NAPLEX Information
An in-depth overview of NAPLEX eligibility, structure, content areas, and prep tips.
NAPLEX Blueprint
A blueprint of the NABP’s NAPLEX competency statement content and distribution.

NAPLEX Study Guide
A comprehensive guide detailing NAPLEX study materials, techniques, and schedules.